Sickle cell disease—a complex genetic disorder1
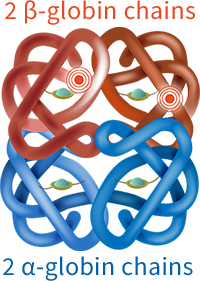
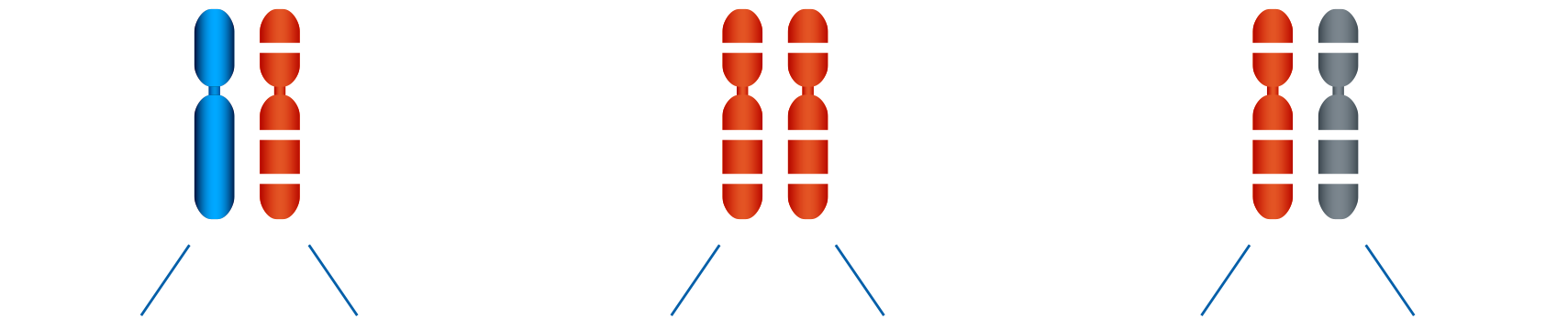
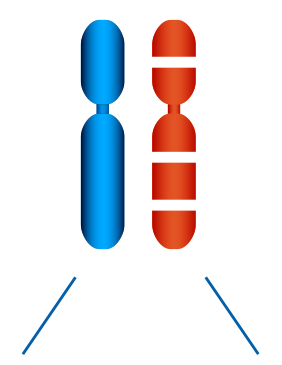
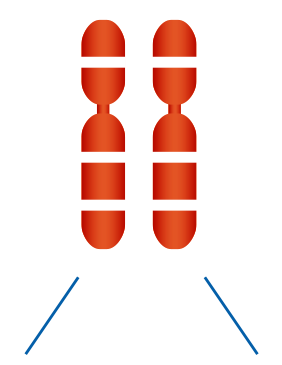
Sickle cell disease (SCD) is a complex disorder that affects the structure and function of haemoglobin, reduces the ability of red blood cells (RBCs) to transport oxygen efficiently, and, early on, progresses to a chronic vascular disorder.