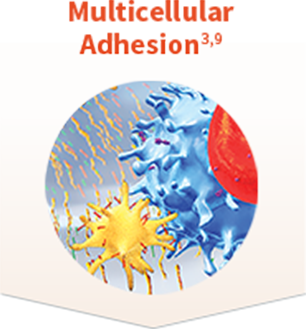
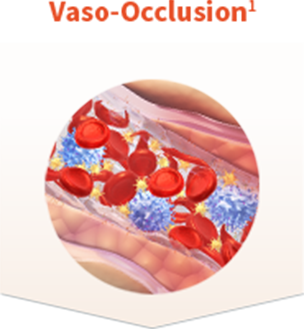
Multicellular adhesion plays a major role in vaso-occlusion and vaso-occlusive crises1,2
Sickle cell disease (SCD) goes beyond red blood cells (RBCs) and progresses to a chronic inflammatory vascular disorder early in a patient’s life.1-3 This chronic inflammatory state leads to increased multicellular adhesion and plays a major role in the pathophysiology of vaso-occlusion and vaso-occlusive crises (VOCs)—the clinical hallmark of SCD.1,2,4