
It has been reported that:
~68% of VOCs are treated at home*
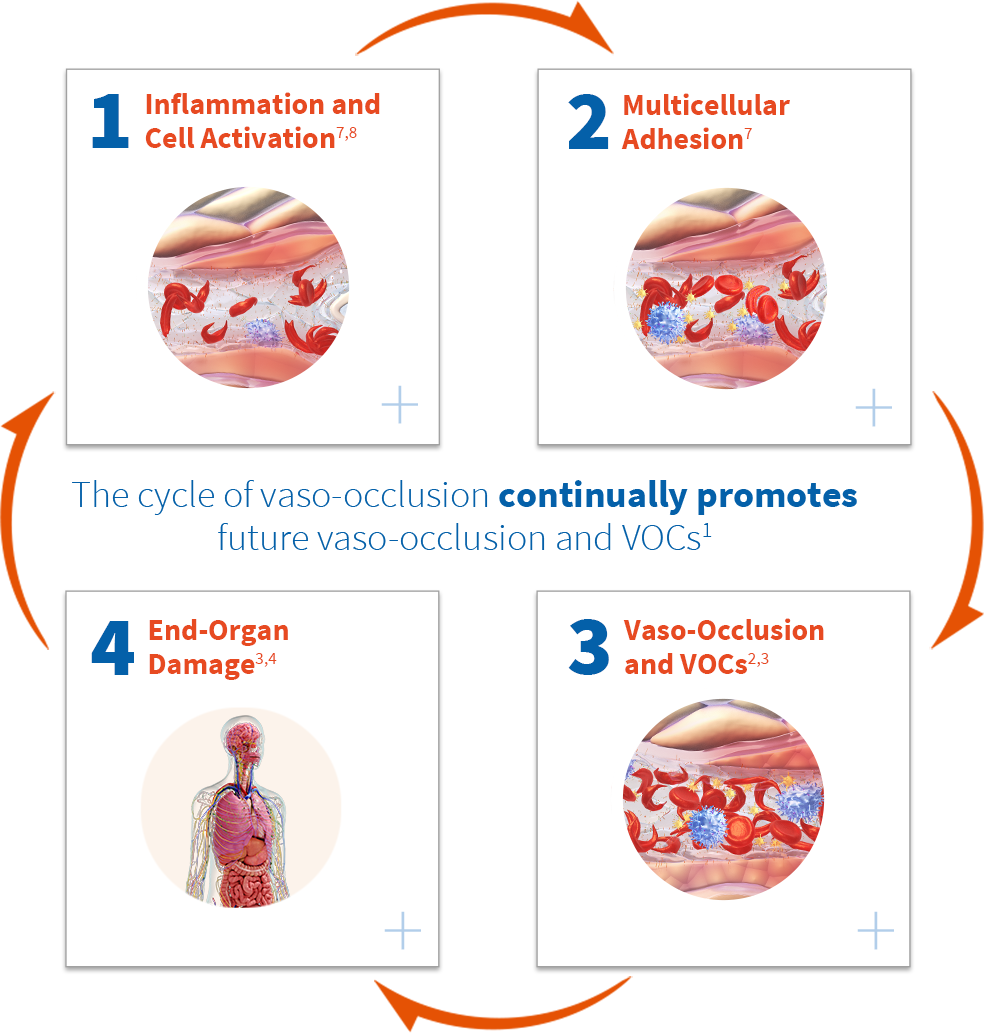
Ongoing and often silent vaso-occlusion can culminate in vaso-occlusive crises (VOCs), the clinical hallmark of sickle cell disease (SCD). VOCs are often unpredictable and painful events that can require medical intervention. 1-3
CLINICALLY VISIBLE
VOCs can be unpredictable, extremely painful events that last, on average, 10 days.3,4
CLINICALLY VISIBLE
VOCs can be unpredictable, extremely painful events that last, on average, 10 days.3,4
SUBCLINICAL
Ongoing and often silent vaso-occlusion occurs systemically during a patient’s lifetime, potentially resulting in acute and chronic complications.3,4
In the Netherlands5

It has been reported that:
~68% of VOCs are treated at home*
In the United States6

It has been reported that:
~79% of VOCs are treated at home†
*Based on the first study of daily pain in a European cohort of patients with sickle cell disease (SCD), in which 55 adults completed twice-daily pain diary logs, home management of pain episodes constituted about 3% of the total days, whereas the use of health care facilities for a pain crisis episode constituted only 1% of the total days.
†According to PiSCES (Pain in Sickle Cell Epidemiology Study), in which 232 adults with sickle cell disease completed daily pain diary logs, home management of pain episodes constituted about 13% of the total days, whereas the use of health care facilities constituted less than 4% of the total days.
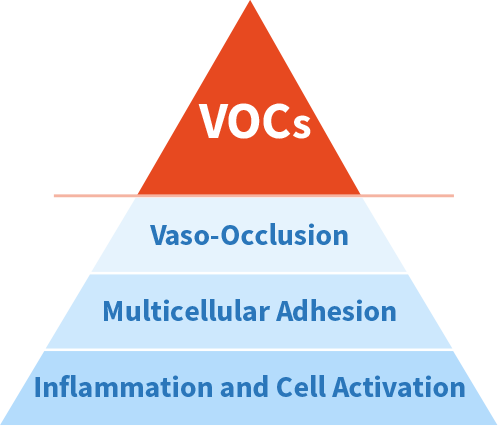
Multicellular adhesion caused by chronic vascular inflammation promotes vaso-occlusion and VOCs.1
References: 1. Conran N, Franco-Penteado CF, Costa FF. Newer aspects of the pathophysiology of sickle cell disease vaso-occlusion. Hemoglobin. 2009;33(1):1-16. 2. Puri L, Nottage KA, Hankins JS, Anghelescu DL. State of the art management of acute vaso-occlusive pain in sickle cell disease. Paediatr Drugs. 2018;20(1):29-42. 3. Ballas SK, Gupta K, Adams-Graves P. Sickle cell pain: a critical reappraisal. Blood. 2012;120(18):3647-3656. 4. Piel FB, Steinberg MH, Rees DC. Sickle cell disease. N Engl J Med. 2017;376(16):1561-1573. 5. van Tuijn CF, Sins JW, Fijnvandraat K, Biemond BJ. Daily pain in adults with sickle cell disease—a different perspective. Am J Hematol. 2017;92(2):179-186. 6. Smith WR, Pemberthy LT, Bovbjerg VE, et al. Daily assessment of pain in adults with sickle cell disease. Ann Intern Med. 2008;148(2):94-101. 7. Zhang D, Xu C, Manwani D, Frenette PS. Neutrophils, platelets, and inflammatory pathways at the nexus of sickle cell disease pathophysiology. Blood. 2016;127(7):801-809. 8. Kanter J, Kruse-Jarres R. Management of sickle cell disease from childhood through adulthood. Rev Med. 2013;27(6):279-287.